Truthout is an indispensable resource for activists, movement leaders and workers everywhere. Please make this work possible with a quick donation.

One voice – mother and child – Kenya. Image: Rodney Rascona (rascona.com)
Kakamega, Kenya – At the Kakamega Provincial District General Hospital, located in Western Kenya, access to adequate and clean water still remains a pipe dream.* Even though the need is critical the hospital, which works with maternity medicine and birthing procedures for women, still lacks an adequate plumbing system for water. These conditions and others are only made worse by frequent and severe water shortages in Kenya.
“One-third of the people in Africa live in drought-prone areas and are vulnerable to the impacts of droughts,” predicted the World Water Forum in 2000.
The Kakamega’s hospital staff admits that problems of water shortages are common. Because of this, women and children are especially vulnerable as they face the destructive effects of unsafe water. “As women constitute the largest percentage of the world’s poorest people, they are most affected by these changes. Children and youth – especially girls – and elderly women, are often the most vulnerable,” says BRIDGE, a research and information program that is part of (IDS) the Institute of Development Studies – Knowledge Services.
With the negative effects of climate change rising, experts predict that the biggest challenge in the coming years for a majority of the world’s people will be the ability to access clean, healthy and safe water. Should access to clean water be considered a human right?
Rights defenders worldwide answer with a strong, “Yes!” Even though the consensus agrees, water figures currently show that resources and water supplies are declining quickly as global temperatures continue to rise and water sources are literally beginning to “evaporate.”
Twenty year old, Hellen Wasiliwa, from the western part of Kenya, had her baby in a public hospital only one month ago. She went to the hospital so her birthing process would be monitored by medical staff for safety and assurance. But things didn’t work out that way. After giving birth she quickly developed typhoid fever, an often fatal waterborne disease, as a result of her exposure, while she was in the hospital, to untreated and unsafe water.
Kenya is currently unable to provide safe drinkable water in many of its hospitals, a condition that is unimaginable in most hospitals today in the developed world. But conditions are shifting. Three fourths of all Kenyan hospitals have inadequate and/or below standard facilities for both drinking water and water used for sanitation and medical needs. Out of 160 medical centers across the country, a staggering 120, currently do not have consistently working plumbing systems. Why? The reasons are varied.
Those who face the greatest impact in Kenya’s shortage of water are children and pregnant women, who’s health conditions are usually compromised during pregnancy and severely compromised during childbirth. According to statistics from the United Nations Development Program (UNDP), adequate water is becoming scarce. More than 2.5 billion people and almost one billion children worldwide live today without any basic sanitation.
Experts in Kenya now warn that common regional water shortages are a serious threat to the health of expectant mothers. Ranked 50th in the world in maternal and child mortality, UNDP statistics show that Kenya has more than 400 infant deaths per 100,000 births. The facts are clear. Climate change, water supply and sanitation play a responsible role in many of these deaths.
Animal Waste / Human Waste
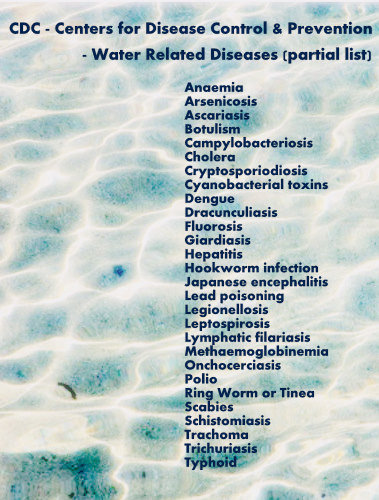
Human contact with polluted water often includes wide exposures to bacteria, viruses and parasites as well as chemical contaminants. The list of dangerous waterborne pathogens is long and extensive. Human and animal waste in water is the most common contaminate. In industrial regions, chemical contaminants are also an ongoing contributor to pollutants.
Hospitals, like Kakamega Provincial District General Hospital, where Hellen Wasiliwa has recently given birth, are often forced to collect rain water in buckets to meet the needs of their patients. Due to severe shortages, the limited water supply is usually shared among patients and is also most often not purified or disinfected. Lack of hospital supplies, proper procedures in sanitation, proper equipment, poor plumbing and facilities, along with less than adequate sanitation training for medical workers and assistants, as well as patient knowledge, contributes to an abysmal mismanagement of water in the region.
Conditions are in a crisis. The dangers of pathogenic contaminants are impacting the operations of hospitals region-wide in Kenya where women and children face the greatest impact. Kakamega township is only one of the areas recovering from a harsh 2009 West Kenya cholera outbreak that claimed hundreds of lives in just one week. Surprisingly, a number regional outbreaks of fatal cases of cholera, “originated in the hospital itself,” explained Dr. Shanaz Sharif, Kenya’s Chief Public Health Officer.
“Typhoid and paratyphoid fever are most often acquired through consumption of water or food that has been contaminated by feces by an acutely infected or convalescent individual or a chronic asymptomatic carrier,” says Eric Mintz of the U.S. CDC – Centers for Disease Control and Prevention.
“After giving birth we had to share (the same) bathing water between seven women,” admits Hellen Wasiliwa describing the days she spent in Kakamega’s hospital. “As a result, I developed a skin rash and got typhoid. I was then re-hospitalized and my bills became very high, despite the poor services. E-coli parasites then began to eat up my internal organs. I almost died,” she said.
Like all other hospitals and health care centers in Kenya, the standard for medical care in Kakamega Provincial District General Hospital is uniquely tied to its relationship to water.

Two young girls carry water on the train tracks that run through the Kibera slum, Nairobi, Kenya. Image: Colin Crowley (newbeatproductions.com)
Rampant Mismanagement
Overcrowded conditions create more risks. As more women patients are admitted than the number of beds allow, stress to many hospitals increases exponentially. In hospitals the price of medical treatment can be prohibitive. A majority of hospital pregnancy wards are still charging more than most poor women can pay, approx $17- $40 USD, just for admitting a woman as a new patient. This keeps many women who may wish to have standard medical services out of hospitals all together.
On top of the fee to admit a patient, a daily bed fee – plus a much higher and separate fee for medical procedures during delivery – keeps women who make less than $2 USD per day far away from any opportunity for medical treatment — unless they are in a critical need. In certain hospitals, those who cannot pay have been known to lay on the floor during their hospital stay while beds go to paying patients.
Finding it difficult to share her experience, Wasiliwa led me from Kakamega’s hospital to her homestead while we talked about her situation. Along the way, she revealed that her newborn son had also developed typhoid as a result of eating food cooked with contaminated water that contained bacteria and parasites.
According to medical evidence, water borne parasites and bacteria can destroy the intestines, resulting in extreme pain and possible death if medical attention is not given immediately. I felt that Wasiliwa, and her newborn, were very lucky to have survived an ordeal that many expectant mothers continuously face.
Some Kenyan rural hospitals have blamed government mismanagement and misappropriation of funds that have been channeled to hospitals in urban, instead of rural, areas as some of the causes for their problems with water.
“The health workers did not seem to care,” continued Hellen as she described the hospital in Kakamega. “At one point, I noticed a nurse laughing at another woman who had just given birth. It was not a nice experience. I and my baby had to be airlifted to Nairobi for additional treatment. I did not have the money but a good Samaritan paid my hospital bill.”
“In Kakamega Hospital, I remember having to share water with a specific fellow patient who had just given birth since the water shortage and drought has been so very severe. She was very weak and sickly. I felt bad, but I had no power to help her. She was then taken to a hospital in nearby Kisumu by air to receive specialized treatment,” said Hellen Wasiliwa.
In 2007, the Kisii District Hospital, in the western Kenya highlands near Kisumu, was down at its lowest level of production. It had zero people receiving safe drinking water. In addition to this, massive problems in hospital management were wrapped in water needs of up to 180,000 litres per day. The hospital had obvious challenges, opened since 1916, it suffered from frequent equipment break downs, along with long periods of time when only enough water to use was saved for “essential services.”
“Non-piped water supplies, such as roof catchments (rainwater harvesting), surface waters and water collected from wells or springs, may often be contaminated with pathogens,” says WHO – the World Health Organization in a May 2009, Guidelines for Drinking Water – Water and Sanitation report. “Such sources often require treatment and protected storage to achieve safe water,” continues the report.
Can Improvements Be Made?
For women, the sub-standard conditions at Kisii Hospital pointed to disaster for those mothers who depended on the medical experience of a hospital setting and were in need of prenatal and neonatal care. Outdoor latrines were used, sheets were not provided for beds, polluted river water was purchased from vendors to use for cleaning and doctors and nurses had little water to use to clean their hands after treating patients.
Today improvements are being made. The picture is drastically changing. Medical health care has improved in the region as concentrated international efforts brought water to Kisii District Hospital from a source that is over one mile away. In 2007, zero people were receiving drinkable water. In 2008, over 3,000 people were receiving drinkable water daily, although there has been much need for expanded improvement of the original hospital building and plumbing as ongoing needs and drought conditions continue to impact the region.
One of Hellen Wasiliwa’s nurses back in Kakamega Hospital, who prefers to remain unnamed, admits that water remains a serious problem at the hospital where she works. To the nurse the problems have appeared because of “mismanaged” funds. “This hospital for some reason has not paid its water bill for the last 6 months,” she said. “As a result, the water connection has been cut off since then. Money that is supposed to be used for (hospital) necessities also has gone to some people’s personal pockets. It is very unfortunate and a grave matter.”
Connection pipes for water at Kakamega Hospital are also in poor condition as the facility needs serious renovations in order to meet proper health standards. Acknowledging Hellen Wasiliwa’s medical woes, the nurse emphasized the severity of the situation since Hellen developed several serious bacterial infections as a direct result of drinking and using unclean water while she was a patient in the hospital.
“Her (Hellen Wasiliwa’s) case was unfortunate. Because of this, we (Kakamega Hospital) have a pending case with the Medical Practitioners and Dentists Board.” The Medical Practitioners and Dentists Board functions partially as a watchdog group to offer Kenyans the most “effective and efficient medical services available” by ensuring medical practitioners (and dentists) are highly qualified in their profession.
“Most of my (hospital) colleagues are under investigation now, including myself,” added the nurse. “The board is wondering why such a situation in a major hospital has gone unreported; even after a cholera outbreak originated from this facility. I do not take responsibility for that, but only time will show the outcome.”
Even with numerous cases of newborn diarrhea that have been charted and still remain high in many regions in East and West Kenya over the years, the government has been slow to curb the trend. In Sub-Saharan Africa, medical treatment for diarrhea is usually given only approx 12% of a hospital’s working budget, as hospitals battle with more than half of their patients who suffer from fecal-contaminate related disease.
After pneumonia, UNICEF statistics show that waterborne diseases such as cholera, amoeba, e-coli and typhoid are the second leading cause of death for children over 5yrs of age. Waterborne disease has been documented as the, “leading cause of death,” among African infants and children who are younger than five years of age.
Due to a growing water shortage and the widespread occurrence of water related disease, pregnancy in Kenya is sometimes seen as a death sentence instead of a blessing for many Kenyan mothers. Increasing scarcity of water and lack of water hygiene continues to present grave challenges for women who give birth, some who do end up dying during or after child birth because of an avoidable break in hygienic safety. The numbers of deaths and the numbers of women and children who have contracted waterborne disease is often not adequately charted or reported.
Forty-Three Percent Without Access to Safe Drinking Water
Pumwani Maternity Hospital, in Kenya’s capital of Nairobi, is the largest maternity hospital in East Africa. As a much more modern facility, it has all the right equipment with an adequate supply of water most of the time. But regular disconnections in the hospital’s water are still common; especially when bills, running in the region of $50,000 USD per month, aren’t paid on time. It’s obvious that water shortage has lead to increases in the price of water, a fate that can cripple the operations of many hospitals.
The situation of water safety is critical. “Forty-three percent of the population of Kenya is without any sustainable access to safe drinking water,” says a 2006 UNICEF Africa report. Because of this the odds against women for safe procedures in hospitals run against them. Maternal mortality is a real and looming possibility even when medical care is supervising. Shortages extend to more than just water. A need for more trained doctors and medical personnel for non-urban Kenyan hospitals is ongoing.
“We need a better understanding of why so many mothers die during child birth,” said former Kenya World Health Organisation Country Director, David Okello.
27 yr old, Jane Kisia, delivered her child at Nairobi’s, urban centered, Pumwani Maternity Hospital only eight days ago. Despite the fact that Pumwani Hospital has adequate facilities , the hospital ward remained without water for more than a week while Kisia was a patient there. Due to these extreme hardships Jane’s newborn daughter developed a life-threatening case of diarrhea.
“My daughter developed serious medical complications,” said Jane. “We called public health officers to the hospital. It was only then when my sanity was restored,” she admitted.
“Last year alone, more than 7,000 Kenyan children (under five years old) died from diarrheal diseases,” said Dr. Francis Kimani, Kenya’s Director of Medical Services. “Most through eating contaminated food and lack of access to basic hygiene and sanitation.”
Water safety implementations are playing a direct and key role in controlling unwanted disease and deaths in Kenya.
Facing Responsibility
“While there is no magic bullet that solves all maternal health problems, the great majority of maternal deaths can be prevented through simple cost-effective measures, which can be implemented even where resources are scarce,” says Women Deliver, an international advocacy organization working to raise reproductive dignity and health for women.
“Yes, there is a history of water shortages in most of the 160 (officially registered) hospitals in Kenya, but we, as a government, are reversing that trend. We are (now in the process of) renovating more than 100 hospitals in the country as the government invests more than 800 million USD for renovating facilities. Aimed at improving medical services, the renovations are extensive and should be complete by mid 2011,” added the Director.
Additional 2011 funds from the World Bank, up to 200 million USD, are planned to help Kenya deal with severe water and sanitation issues in numerous health institutions across the country. At the same time, Kenya’s Health Ministry is also raising additional funds to help implement the project. Other NGOs like The Rotary Club (Colorado, U.S.) are helping individual hospitals, like the Kisii District Hospital near Kisumu, where sagging plumbing systems are coming up to standards as they help get water “on the agenda.”
“Sewage contaminated water used for drinking, washing or preparing foods, is a significant form of indirect transmission, especially for gastrointestinal diseases such as cholera, rotavirus infection, cryptosporidiosis and giardiasis,” says a recent 2010 report by the U.S. based leader in the field of science education, the BSCS – Biological Sciences Curriculum Study, that currently works under the U.S. National Institutes of Health and the National Institute of Allergy and Infectious Diseases.
Like countless other women in Kenya, as a mother of three, Hellen Wasiliwa, continues to face the challenge of living in an environment where low water hygiene and “climate change provoked” water scarcity surrounds her. She is not the only one impacted by this. In her own household she lives together with her extended family — including her parents and other relatives.
Even though Hellen has given birth recently she has little time to rest and regularly makes a two hour trip, each way, to fetch water for her household. When she reaches her destination the water she gathers is in decline and often unsafe for drinking.
________________________________________________________________________
Climate change expert, Anabell Waititu, from the Institute for Environment and Water – Kenya and the Gender and Water Alliance, outlines Kenya’s water shortage crisis and its impacts on women during the COP14 – Copenhagen Climate Talks Conference 14 in Poznan, Poland, December, 2008. What does it take to get legislations to include women and gender inside important key problem solving discussions on global water?
________________________________________________________________________
For more information on this topic:
- “Gender and Water – Mainstreaming Gender Equality in Water Hygiene and Sanitation Interventions,” SDC – Swiss for
- Development and Cooperation, Federal Department of Foreign Affairs (FDC), August 2005
- “Kisii hospital water supply funding study – Peer Water Exchange,” 2007
- “Focus on 5 – Women’s Health and the MDGs,” Women Deliver, April 2010
- “Water, Sanitation and Health – Microbial Aspects,” World Health Organization, May 2009
___________________________________
Women News Network – WNN correspondent from Nairobi, Gitonga Njeru, a recent recipient of an award grant from The Fund for Investigative Journalism in Washington, D.C., is a journalist who specializes in investigative stories, climate change, rights issues and science reporting. His material for news stories has been published by Reuters News AlertNet, The Guardian (UK) and Africa Science News, along with The Daily Nation and The Nairobi Star Newspaper in Kenya. Njeru’s work has also been featured by Spore Magazine (Brussels) and Ooskanews (US) covering water, land and sanitation conditions in developing countries.
A veteran of countless projects in all hemispheres, photojournalist, Rodney Rascona, is committed to using his experience gained from a decade of covering famine in Ethiopia, the global food crisis in Kenya and vital AIDS/HIV education to play his part in easing the human condition. His career highlights include acting as chief photographer for a major non-governmental organization (NGO) for 11 years, being a founder of HEART, a medical program that enables children in the developing world to have life-saving heart operations, and working the 2004 tsunami fields in India/Indonesia. His latest photographic project, “The Pink Door Photographs“, produced for multiple relief organizations, is a premiere exhibition created to generate funds and raise continued awareness for the earthquake-shattered Haitian community. At the core of his work, Rodney creates images of consequence. His unusual breadth of life experiences coupled with compassion lends his subjects a clear and powerful voice. Through his photographs, he becomes their advocate and lifts the veil, giving a rare glimpse into the lives of people who live just beyond the realm of our own life experience. For more information on him and his work connect HERE.
Photojournalist, Colin Crowley’s, past projects have taken him from the deserts of Afghanistan, into earthquake-ravaged cities in Pakistan and through the slums of Nairobi. In 2005, Crowley covered an inside look at the education system in Afghanistan by covering a school in Kandahar, Afghanistan. He also covered the 2005 earthquake in Pakistan and the people of Tajikistan for the international NGO, Shelter for Life (SFL). Currently Colin is working for the UK based NGO, Save the Children, getting coverage on the China earthquake, the Myanmar cyclone, the ongoing war in DR Congo, the cholera outbreak in Ethiopia, food crisis in Northeast Kenya and humanitarian needs in South Sudan and Haiti. For more information on Colin Crowley and his work link HERE.
/Additional research material for this story has also been provided by Lys Anzia, 2006 Pushcart Prize nominee, journalist and editor-at-large for WNN./
__________________________________
Additional sources for this article include WHO – the World Health Organization, UNDP – United Nations Development Programme, Kenya World Health Organisation, Kenya Ministry of Public Health and Sanitation, Department of Health Sciences – Gusii Institute of Science and Technology, BRIDGE & (IPS) the Institute of Development Studies – Knowledge Services, Department of Clinical Pathology – Kenyatta University, UNICEF – United Nations Childrens Fund, Africa Renewal magazine, Women Deliver, U.S. National Institutes of Health, The National Institute of Allergy and Infectious Diseases, Peer Water Exchange and the CDC – U.S. Centers for Disease Control and Prevention.
_________________________
©2010 Women News Network – WNN
A terrifying moment. We appeal for your support.
In the last weeks, we have witnessed an authoritarian assault on communities in Minnesota and across the nation.
The need for truthful, grassroots reporting is urgent at this cataclysmic historical moment. Yet, Trump-aligned billionaires and other allies have taken over many legacy media outlets — the culmination of a decades-long campaign to place control of the narrative into the hands of the political right.
We refuse to let Trump’s blatant propaganda machine go unchecked. Untethered to corporate ownership or advertisers, Truthout remains fearless in our reporting and our determination to use journalism as a tool for justice.
But we need your help just to fund our basic expenses. Over 80 percent of Truthout’s funding comes from small individual donations from our community of readers, and over a third of our total budget is supported by recurring monthly donors.
Truthout’s fundraiser ends tonight! We have a goal to add 122 new monthly donors before midnight. Whether you can make a small monthly donation or a larger one-time gift, Truthout only works with your support.