Part of the Series
Fighting for Our Lives: The Movement for Medicare for All
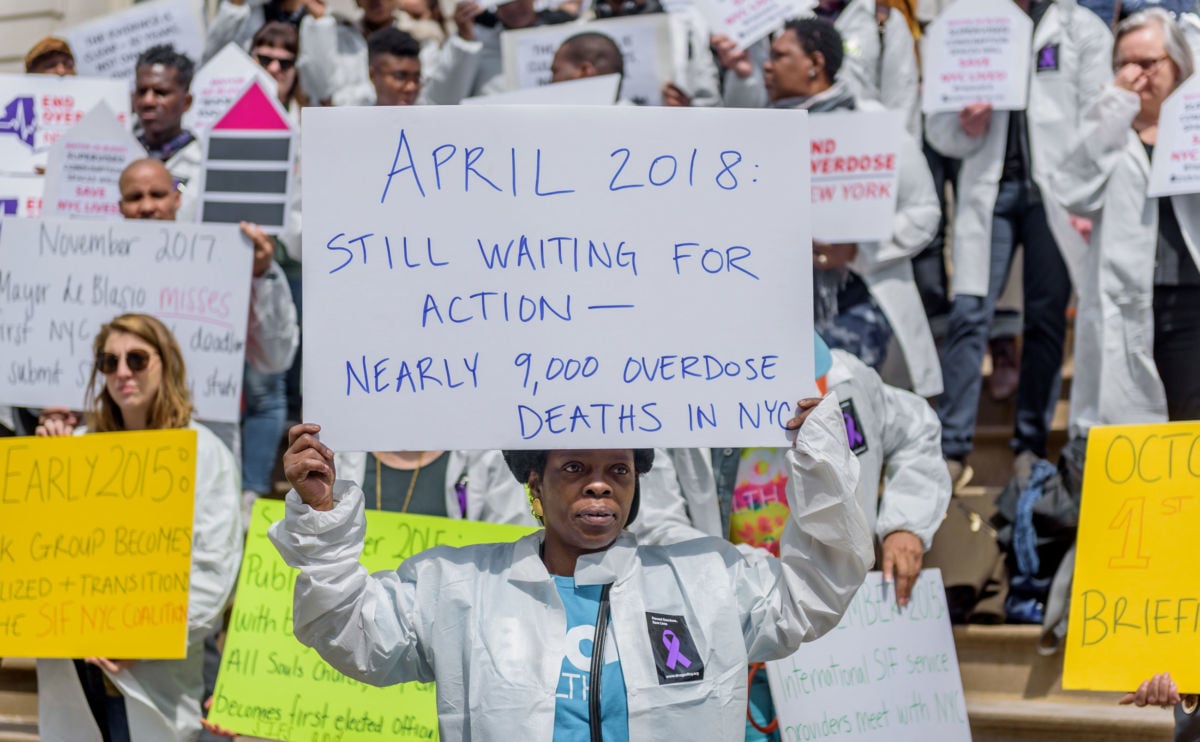
It is widely expected that by Election Day Donald Trump will sign the Support for Patients and Communities Act or opiate bill (H.R.6), that was finalized by Congress on October 3. There will surely be fanfare when the bipartisan bill — passed 99-1 in the Senate — is signed into law. The opioid crisis kills 115 people a day and has touched Americans everywhere. The Mayo Clinic calls it the “most important and most serious public health crisis” today. “We’ve stepped up to the plate,” boasted Sen. Shelley Moore Capito (R-West Virginia), seemingly pleased she could tell her voters that Congress took action.
The reality, however, is that the bill is woefully insufficient given the scale of the problem, according to a strong consensus of public health advocates. There are valuable provisions, but it is largely, as Rep. Peter Welch (D-Vermont) lamented, “a very energetic effort to pretend we’re doing something significant.”
The bill largely focuses on “supply side” enforcement. This includes an effort to stop fentanyl, the potent opiate that has caused a sharp spike in overdoses, through law enforcement and interdiction. It also encourages the development of non-opioid pain medications and launches a competitive grant-based pilot project for people transitioning to independent living.
The legislation also raises the cap on how many patients a doctor can prescribe an important treatment. Most doctors who are trained to prescribe buprenorphine (Suboxone) are limited to 100 patients, but under the new law, they could have 275. Medicare will also now cover methadone. In the past, methadone was not covered because it isn’t usually dispensed in a retail pharmacy, a requirement for Medicare Part D.
Many of these reforms are welcome, advocates say, but the bill does not do enough to expand treatment for people who need help now.
“The bottom line is, we need people to be alive if we want to help them,” said Nancy Nielsen, senior associate dean of health policy at the University of Buffalo, in an interview with Truthout.
Why Medication-Assisted Treatment Matters
Methadone and buprenorphine are considered the most effective treatments for chronic opiate abuse disorder. The medications are “partial opiate agonists,” meaning they do, like any opiate, bind to opiate receptors. The medication does not, however, provide euphoric effects for opiate-tolerant individuals. It also binds so strongly to receptors that it serves to block or minimize the effect of full opiates like heroin or oxycodone.
There is widespread consensus among public health experts that these medications are the most effective treatment for chronic opiate abuse. Evidence supporting the use of the medications are found in clinical guidelines and reports from the Substance Abuse and Mental Health Services Administration, the National Institute on Drug Abuse, and the Centers for Disease Control and Prevention, among others. Methadone and buprenorphine are especially important during an overdose epidemic since they can lower mortality rates by between 66 percent and 80 percent, as reporter Zach Siegel outlined at Slate. “We know how to treat opioid addiction,” he said, “but our antiquated conceptions of addicts prevent us from doing so.”
Advocates insist that making these medications available should be central in response to the crisis, and the new opiate bill falls far short of what is needed.
“We have treatment that works. The priority should be making it so anyone who wants help can go see a doctor or an ER and get on medication-assisted treatment,” said Bruce Trigg of the Harm Reduction Coalition. “We know of ways to help make this happen but Congress is not thinking big, not wanting to spend money.” The opiate bill has not been scored by the Congressional Budget Office, but the Senate version contained about $8 billion in new spending.
In a sense, this disappointment was inevitable. This is the United States: health care is a commodity, patients are “consumers.” It would be inconsistent to solve the grave opioid crisis by providing widespread coverage for vulnerable populations. A public, government-led expansion of care is a nonstarter for most of the GOP. There are an increasing number of Democrats embracing these policies, especially in the House. But the 115th Congress is still a very conservative body controlled by politicians who have been hell-bent on taking health care away from Americans.
After all, if enough members of Congress cared about moral, humane health policy, the US would probably already have a universal, national health system that was designed to put patient needs first. The US doesn’t have a health care “system” so much as a jumbled mess that makes a coherent national response to the opioid crisis essentially impossible. This is something advocates of a single-payer system point out.
“Single-payer makes health care about the patients. Our health system currently has nothing to do with patients. It is all about profit,” Trigg said.
Indeed, this crisis is very much rooted in greed. Pharmaceutical companies have been lobbying to make sure they are taken care of in the final bill. This profit motive is a major reason why the drug industry helped start (and is still profiting from) the epidemic. Under a single-payer Medicare for All system, which is supported by 70 percent of the country, the incentives would be different.
“In theory, you could have a single-payer system that negotiates drug costs but continues to allow pharma to market directly to patients [and] pay off and deceive physicians,” said Benjamin Day, director of Healthcare-NOW, in an interview with Truthout. “But, there’s a reason you don’t actually see that anywhere in the world — once you have a single-payer system, any policies that actually make people sicker you have to pay for down the road, so such systems naturally create incentives for preventive care and policies.”
In fact, the opiate crisis is a very “American problem,” as the BBC notes. In Europe, where health care is a right under international treaties, the opiate problem is not nearly as bad. The US has around 4 percent of the world’s population but about 27 percent of the world’s drug overdose deaths, according to the United Nations Office on Drugs and Crime. Notably, the US is also one of only two countries that allow prescription drugs to be advertised on television.
You will find more infographics at Statista.
Canada has a serious opiate problem, but not as extreme as in the United States. Interestingly, in Canada socialists have been trying to help, in part, by creating (sometimes unsanctioned) injection sites and building solidarity. Both countries have relatively weak welfare states and high inequality. (Canada’s health care system is understandably praised by Americans, but Canadian advocates note that the Canadian system is the only universal health care system without drug coverage.)
Federal Government Lags Behind
Overhauling how we finance health care is not the only change that must be made to confront the opioid crisis. There are many valuable tactics being used by county and state officials that help. But the tools are largely being ignored at the federal level and are largely absent in the new bill, Trigg said.
Some hospitals, for instance, will now offer patients medication-assisted treatment if they go into an emergency room for an opiate-related issue, such as an overdose or a withdrawal. Patients who come in with an overdose are also of a great deal of importance since about 7 percent of overdose survivors die within a year.
“We have these people who need help in the door, for whatever reason, and for years we have been tossing them to the street,” Trigg said. “It just doesn’t make any sense. They go out and within a year many of these people are dead.”
Nielsen notes that she is involved in a program in Buffalo that offers similar services. “Someone comes into the emergency room — might have been an overdose or an abscess or any number of things — and if they want help we have 13 hospitals that will give them a prescription that day,” Nielsen said. The program provides training to help doctors get waivers as well.
Some jails and state prisons have been increasingly offering various forms of medication-assisted treatment, though, of course, not nearly enough of them. Rhode Island is currently the only state prison system to offer all three of the major medications (buprenorphine, methadone and naltrexone) to prisoners, Trigg said. He noted that the federal prison system, in particular, offers very few opportunities for medication-assisted treatment (as Mike Ludwig has ongoingly reported for Truthout). Medical neglect is especially rampant in the world of corrections and law enforcement, and a lack of access to medication-assisted treatment is no exception.
“It is a wasted opportunity. You have all these vulnerable populations in these jails. Most of them probably don’t deserve to be there, but while they are there we should at least offer them treatment,” Trigg said.
The United States jails more people per capita than any other country on the planet, and 65 percent of prisoners fit the criteria for substance abuse disorder. Yet only 11 percent are given treatment (and those treatment options are often very limited). Outside of prisons, only 22 percent of people who qualify for the clinical definition of substance abuse disorder treatment receive treatment. Though not all of that is due to lack of treatment options, the most common reason for not getting treatment is cost (cited by 39 percent), according to a survey from the National Survey on Drug Use. A 2017 study published in the Annals of Family Medicine found that about 60 percent of rural counties in the United States (where much of the epidemic is located) don’t have a single physician who has a DEA [Drug Enforcement Administration] waiver to prescribe buprenorphine.
People on probation or parole may be denied treatment (or forced to taper off medication) by their probation officers, a practice which may violate discrimination laws aimed at protecting those with mental illness, according to the Legal Action Center. Congress has done nothing to eliminate these obstacles.
Constant Barriers Push People Away From Treatment
Eliza Tartell is a single mother of one who lives in Cape Cod and knows these kinds of barriers all too well. The area she lives in has been hit especially hard by the ongoing overdose crisis. It was called a “shoreline of addiction” by the Guardian as recently as May and the subject of a documentary as well. Tartell has been living with opioid abuse disorder and PTSD for much of her life, and she wants help.
Despite being insured and living in Massachusetts, a state that has more access to evidence-based treatment than most, Tartell tells Truthout she has continually been denied and/or dismissed when trying to get buprenorphine treatment for a variety of reasons. One time she was not given treatment due to a pregnancy (denying medication-assisted treatment based on pregnancy conflicts with protocols made by the American Society of Addiction Medicine).
“I’ve been sent away so many times because the doctor has too many patients,” said Tartell in an interview with Truthout. “I [have] had to commute hours and hours for weekly treatments that were nearly impossible…. I have been denied care because of my psych meds.”
Most recently, she dealt with two closures of outpatient suboxone programs at Arbour, the largest for-profit mental health provider in the state, within one year. She tried to transition into a different facility in Cape Cod, but they closed their outpatient program as well. Another provider refused to help her because of the medications she takes for anxiety and PTSD. After these denials, Tartell was left feeling panicked and overwhelmed with fear and frustration.
“My options were relapse or hospitalization, and I have a kid I need to take care of.” she said.
Out of reasonable options, she says, Tartell was forced to go off her medication and is attempting to stay off opiates without medication-assisted treatment. This is risky. “Retention in methadone and buprenorphine treatment is associated with substantial reductions in the risk for all cause and overdose mortality in people dependent on opioids,” concluded a study in the BMJ from 2017.
Doctors’ hesitancy to treat people on benzodiazepines (anxiety medication) may well be guided by a 2016 FDA warning that urged caution when mixing these drugs and medication-assisted treatment. But they have since updated that warning as evidence showed refusing treatment to these patients is significantly more dangerous than co-treating patients with both medications (which increases risk of respiratory depression but not in a statistically significant way, according to the FDA’s follow-up advisory). “The dangers associated with failing to treat an opioid use disorder can outweigh the risks of co-prescribing MAT [medication-assisted treatment] and benzodiazepines,” the FDA concludes.
In fact, only 322 deaths were reported to involve buprenorphine in 2014, despite the sinister media coverage of the drug, including The New York Times’s infamous “Treatment With a Dark Side,” article in 2013.
“My biggest regret as a doctor was, when I started prescribing buprenorphine 10 or 12 years ago I used to tell people with anxiety medication in their system to clean their system out and come back,” Trigg said. “But some of those people will never come back once you show them the door. And some of them will die.”
In some parts of the country, lower-income people face a massive barrier to ongoing medication-assisted treatment: 11 states have lifetime caps after which Medicaid stops paying for medication-assisted treatment after one or two years. In some states prior authorization may enable the treatment to continue — another barrier.
Given the nature of the treatment, time limits are a critical problem. The FDA’s guidelines instruct that “patients may require treatment indefinitely and should continue treatment for as long as they benefit and as long as the use of [medication-assisted treatment] contributes to their intended treatment goals.”
Sadly, the bill that Congress has passed, and which Trump is expected to sign soon, does very little to help Tartell and others in her situation. Even the best parts of the bill have limited utility, Trigg notes.
“It is great to allow doctors to see more patients and prescribe them medication,” he said. “But that doesn’t help if doctors are not getting trained, getting the waivers and taking these patients. And a lot of doctors don’t want these patients. The care can be costly, high-maintenance and more time-consuming.”
The Affordable Care Act mandates mental health and addiction as Minimum Essential Benefits, but it gives each state wide latitude to determine what coverage means. Some states cover medication-assisted treatment, others do not. Some states have lifetime caps or dosage limits and others do not. Some states cover inpatient detox, but not counseling. Other states do the reverse.
“The system is just so complicated. There are federal rules and restrictions and some states add their own, more strict regulations,” Trigg said, noting that medication should be easily accessible to all who need it.
If the US implemented an integrated, universal health care system, someone like Tartell would be in much better shape. When her treatment center closed, it was a decision made for financial reasons to serve the interests of board members of Arbour’s parent company who were located hundreds of miles away in central Pennsylvania. If patients were a priority over profits, this is not how business would be done, and Tartell would be less likely to keep running into (very sudden) closures.
Of course, even with a single-payer system that put patients first, there are still barriers created by stigma — from providers, from the community, and even from some aspects of the recovery community. So, a push toward national health care reform must also include efforts to educate providers, families and communities about ending stigma.
Lessons in Clinical Neglect and Human Folly
The medical term “iatrogenesis” describes a scenario in which injury or illness occurs because of medical care. It is from the Greek, meaning “brought forth by the healer.”
“It is a great word to describe the crisis,” Trigg said. “Drug companies, providers, physicians, policymakers — there is a lot of blame to go around.”
Indeed, the term can be used accurately to describe many historical efforts at practicing medicine. Until the 19th century, there was near-global consensus in favor of Humorism — a practice that involved bleeding patients to maintain the right balance of, “blood, phlegm, yellow bile and black bile.” This nonsense was the mainstream treatment for 2,000 years and not discarded entirely until the mid-19th century. It led to widespread bloodletting as treatment for countless ailments.
Humorism died in the 19th century as the scientific revolution occurred. But the fact that this pseudoscience survived two millennia should humble us all. Humanity is capable of wide-scale clinical negligence. In many ways, the US approach to the opiate crisis is more negligent because, unlike the doctors who practiced bloodletting in the 15th century, we have a solid grasp of the science of opiate abuse disorder and how to treat it. But the greed inherent in the market-based health care system of our capitalist society has many policymakers and providers ignoring evidence.
The federal government’s weak response to the opioid crisis is a sad contemporary example of this folly. More than that, it reflects one of the US’s true national tragedies: its lack of a national health system that prioritizes patients above all else. So long as greed is at the heart of American medicine, the country will face more tragedies like this opiate epidemic.
Join us in defending the truth before it’s too late
The future of independent journalism is uncertain, and the consequences of losing it are too grave to ignore. To ensure Truthout remains safe, strong, and free, we need to raise $31,000 in the next 48 hours. Every dollar raised goes directly toward the costs of producing news you can trust.
Please give what you can — because by supporting us with a tax-deductible donation, you’re not just preserving a source of news, you’re helping to safeguard what’s left of our democracy.