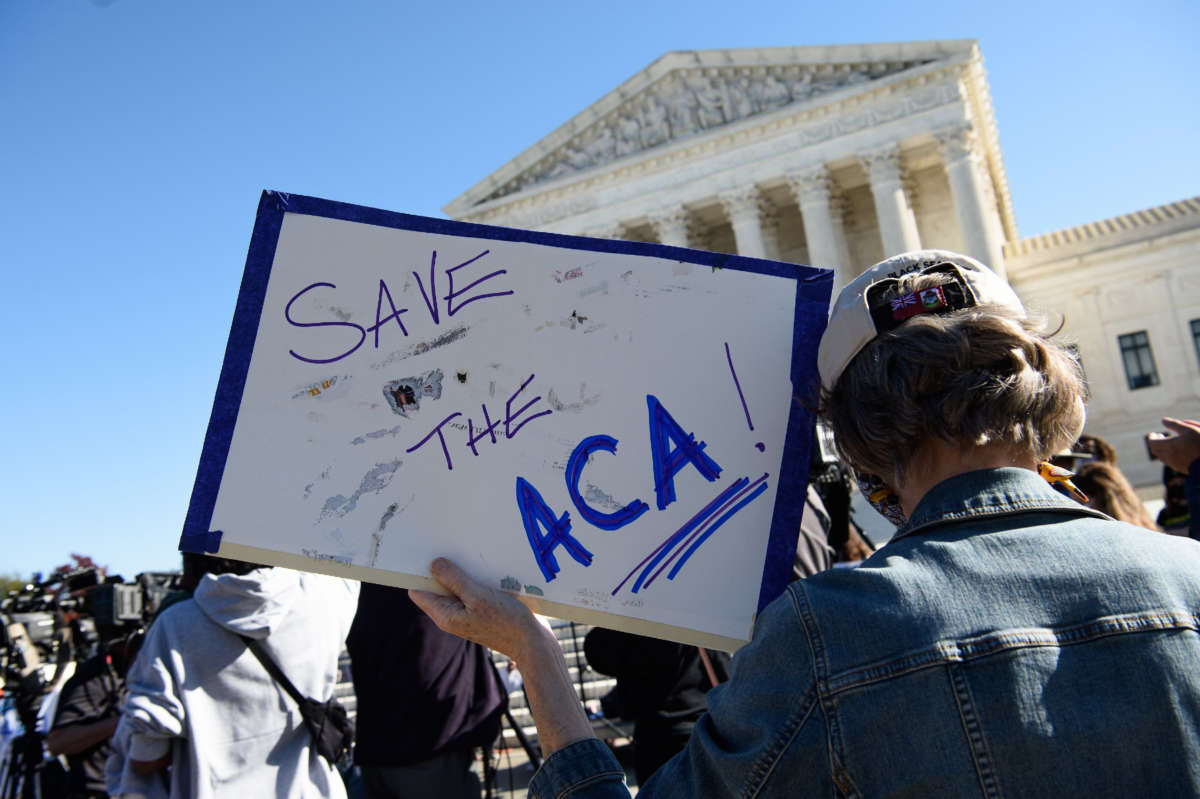
A proposed Trump Administration rule would undermine the Affordable Care Act (ACA) and could cause many people to lose health coverage. If finalized, the Notice of Benefit and Payment Parameters (NBPP) for the 2022 coverage year would encourage privatization of core functions of the health insurance marketplaces, starve HealthCare.gov of needed funds, codify Administration efforts to waive important parts of the ACA, and continue a policy that raises premiums and cost-sharing. Comments on the rule are due December 30 and can be submitted here.
Encourages Privatization of HealthCare.gov Functions
The proposed rule doubles down on the Administration’s November 1 approval of Georgia’s marketplace privatization waiver by letting any state follow suit without a waiver. Under Georgia’s 1332 waiver (named after section 1332 of the ACA), the state will leave HealthCare.gov and require its marketplace enrollees to enroll exclusively through private web brokers or insurers.
This scheme will reduce coverage among the 500,000 Georgians who now enroll through HealthCare.gov, without a broker. For starters, many people will likely fall through the cracks in this massive change due to confusion about the new process. That’s what happened in states that shifted from the federal marketplace to a state-based marketplace or vice versa, a transition much simpler for consumers than what Georgia is attempting.
Also, consumers will lose access to HealthCare.gov’s apples-to-apples plan comparisons. Instead, they’ll have to rely on profit-driven entities, which can withhold essential information (like premiums and deductibles) for plans that don’t pay them commissions, forcing consumers to do significant legwork if they want to explore those options. And these entities sometimes steer people to short-term and other subpar plans and discourage Medicaid enrollment.
By encouraging more states to follow Georgia’s lead, the NBPP would likely cause more loss of coverage and divert more people to subpar plans.
The NBPP would also encourage enrollment assisters and navigators to use enhanced direct enrollment (EDE) websites – websites from private brokers authorized to directly enroll people in marketplace plans – instead of HealthCare.gov and let EDE websites operate for up to a year without meeting marketplace requirements for presenting materials in languages other than English.
Proposes Additional Harmful Changes
The NBPP also would:
- Cut funding for HealthCare.gov. The NBPP would slash, by 25 percent, the user fee on insurers that helps fund HealthCare.gov operations. This would compromise support for the enrollment website and call center, marketing, outreach, and enrollment assisters, potentially reducing enrollment and undermining customer service ― which could push more states to privatize their marketplaces.
- Promote state deviations from ACA protections. The NBPP would codify parts of 1332 guidance from 2018, which weakens consumer protections by opening the door to waivers that would promote enrollment in short-term plans that lack the ACA’s protections for people with pre-existing conditions, as well as waivers that would reduce benefits or increase deductibles and cost-sharing. The guidance likely violates the ACA’s statutory “guardrails,” which prevent 1332 waivers from reducing coverage or making coverage less comprehensive or less affordable, but codifying it as a rule would make it harder for the incoming Biden Administration to immediately roll it back.
- Continue a policy that raises premiums and cost-sharing. The Administration’s 2019 change in the formula used to calculate premium tax credits, which cut financial assistance for millions of people, would continue under the NBPP. And it would have an even greater impact in 2022, raising premiums by 4.7 percent for most subsidized marketplace consumers after accounting for their tax credits (compared to about 2.7 percent this year). That amounts to a $360 annual premium increase for a family of four with $80,000 in income. The same formula change also increases the limit on consumers’ total out-of-pocket expenses, which applies to both marketplace and employer plans. In 2022, that limit will be $400 higher for an individual, and $800 higher for families, than if the 2019 change were reversed.
Join us in defending the truth before it’s too late
The future of independent journalism is uncertain, and the consequences of losing it are too grave to ignore. To ensure Truthout remains safe, strong, and free, we need to raise $34,000 in the next 72 hours. Every dollar raised goes directly toward the costs of producing news you can trust.
Please give what you can — because by supporting us with a tax-deductible donation, you’re not just preserving a source of news, you’re helping to safeguard what’s left of our democracy.